Gallbladder

Dr Edward Tong has performed over 500 operations to remove a Gallbladder. This is usually done with a keyhole operation. The patient will be given a full general anaesthetic. There will be 4 small cuts – one over the umbilicus and 3 under the rib cage.
Not all patients who has Gallstones need an operation to have their Gallbladder removed. Those patients in whom should have their Gallbladder removed include those who have pain consistent with coming from their Gallstones, those who have had pancreatitis also, those who previously has a stone go into the common bile duct and those who previously have had to go into hospital with an infection of their Gallbladder.
The decision to have the gallbladder removed requires a specialist review which Dr. Edward Tong can offer and this takes into consideration a number of factors including i) the indications for surgery ii) the severity of symptoms and iii) the patients fitness for an operation.
Although removing the Gallbladder is a safe and a very commonly performed operation, it is not without risk of potential complications. Risk of injury to bile duct is quoted at approximately less than 0.5%. Risk of other major complications is quoted at less than 0.1% including bowel injury, hemorrhage and anaesthetic complications.
For most patients, they will require one overnight stay at the hospital. It is not uncommon to have some shoulder tip pain during the recovery phase of the procedure which can take up to 2-4 weeks.
Skin Lesions

Dr. Edward Tong offers where appropriate in the clinic excision of skin lesions at very competitive rates. However, if the skin lesion is too large or in a location such as over the anterior neck – it is possible that Dr. Tong may refer you to a specialist plastics surgeon where it may be a done under a general anaesthetic.
Commonly treated lesions include:
- Lipomas – These are benign proliferation of fatty tissue that presents as a subcutaneous mass. Where it is relatively small < 3cm and relatively superficial – these may be appropriate to be excised in the clinic under local anaesthetic.
- Epidermoid Cysts – These are benign cysts which contain keratin material and often has a punctum overlying the cyst. These cyst can often get infected and subsequently become an abscess. The best time to have these skin lesions excised is when they are not infected.
- BCC- These are skin cancers arising from the basal cells of the skin. Treatment of these skin cancers will require a 2mm margin of normal tissue.
- SCC – These are cancers arising from accelerated growth of squamous epithelium. Dr. Tong offers clinic treatment of these cancers but they also require a 5mm margin of normal tissue.
Complications that can arise from the excision of these skin lesions include wound infections and/or hematoma.
Hernia Surgery

Common hernia that is treated in this practice include umbilical hernia and inguinal hernia. Dr. Edward Tong will address these herniae with an open technique, and this may sometimes involve the insertion of a mesh.
Open umbilical Hernia Repair
These hernia occur through a weakness through the umbilicus (belly button). Contents that can arise include preperitoneum fat, omentum or bowel. Patients usually present with a lump, or with pain. They can also present with an acute bowel blockage if bowel becomes caught up within the hernia sac.
Repair of the umbilical hernia is done under a general anaesthetic. There will be a transverse incision overlying the hernia. The hernia contents are reduced and the defect is closed. The closure of the defect may be done with only sutures or depending on the size of the defect – it may require a mesh.
Complications that can arise from this operation include bowel injury, bleeding, wound infections. There is a risk of hernia recurrence is variable depending on the patient and the size of defect, but it can range from 2-10%.
Open inguinal hernia repair
These hernia occur through a weakness through the inguinal space and can present wither as pain or a lump in the groin. Contents can include preperitoneal fat, omentum or bowel. If bowel becomes incarcerated in the inguinal hernia sac then that becomes a surgical emergency.
Repair of the inguinal hernia is also done under a general anaesthetic. This is done via a groin crease incision. The hernia sac is separated from cord structures, and the content is mobilised and reduced. The defect is closed with a prolene mesh
Complications that can arise include bowel injury, bleeding and wound infection. The hernia can recur and the risk of that is between 1-5%.
Bariatrics
Dr. Edward Tong offers initial assessment and a discussion of options to facilitate weight loss. They can be broken down into non-medical, medical and surgical options. It is important that a thorough discussion looking at all the different options is offered to the patient. Generally speaking, weight loss surgery is only a tool. The success of any treatment regime really depends much more so – on patient compliance to the treatment suggested by the practice. This practice only will offer a laparoscopic sleeve gastrectomy to assist in weight loss.
In patients who are fit for surgery the following patients can be considered for bariatric surgery:
- BMI of 40 or greater
- BMI of 35 or greater with a significant health condition that can be improved with weight loss (eg: Sleep Apnoea, Hypertension and Diabetes)
- BMI 30-35 (with poorly controlled Diabetes)
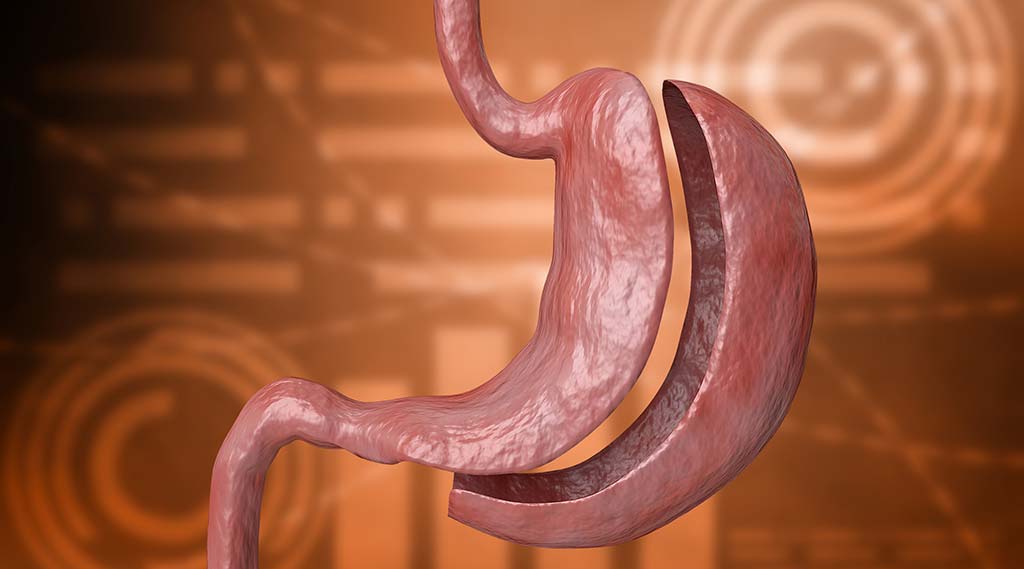
A laparoscopic sleeve gastrectomy is a key hole procedure whereby the stomach is shaped so that is a narrow tube. It works by essentially 2 mechanisms. Firstly, there is a degree of restriction with a stomach that is smaller. Secondly, there is reduction of hunger secreting hormone namely leptin, and hence patients will full more full faster, eating less.
Complications that can arise include a leak from the sleeve which is reported at about 0.5-1%. The staple line can also bleed and it is possible to narrow the stomach tube too much to cause difficulty with eating.
After the operation, patients will likely need to stay in hospital for about 2 days. After the operation, they may need to be on a fluid diet for 2 weeks, and subsequently a pureed diet for 2 weeks after. Close collaboration with a dietitian is necessary in order to optimise clinical outcomes including weight loss.
